How the Biden Administration Is Enabling Hospitals to Violate Price Transparency Requirements
KEY FINDINGS
- The Centers for Medicare & Medicaid Services (CMS) is providing substantial deference to hospitals on price transparency requirements.
- Price transparency enforcement timeframes by CMS are wildly inconsistent.
- CMS is stonewalling access to hospital price transparency records.
Overview
No sensible homebuyer would make a down payment without knowing the price of a home. No responsible driver would take out an auto loan without understanding the price of the car. Yet most Americans have no idea about what their price would be for major surgery at a hospital.
In all facets of life, Americans expect to know prices ahead of time. Yet in health care, this expectation has been cast aside by a system built on opaque prices.
In 2019, the Trump administration sought to change this by issuing a new rule to require hospitals to post an easy-to-use file of charges for different procedures on their website and to display shoppable health care services in a consumer-friendly format.1 Despite strenuous objections from special-interest groups and a lawsuit filed by the American Hospital Association, the rule was implemented in 2021.2

But in 2022, a Foundation for Government Accountability (FGA) review of more than 6,400 hospitals found that nearly two-thirds were not complying with price transparency requirements.3 More recent records suggest that most hospitals are still not compliant today.4 Other organizations have suggested as many as 75 percent of hospitals are ignoring the price transparency rule.5 The Biden administration has come under fire from lawmakers for failing to enforce the rule with publicly accessible information, with one member of Congress noting that, “we can get more information about a local restaurant from Yelp than you can get about your local hospital from CMS.”6
Thousands of pages of new records obtained by FGA have shined a light on precisely why so few hospitals are compliant with price transparency requirements. These CMS records—which include detailed warnings, notices of violations, corrective action plan requests, and monetary penalties—span more than 250 hospitals in 46 states and Washington, D.C. The conclusion drawn from the records is clear: CMS simply does not take price transparency seriously.
CMS is providing substantial deference to hospitals on price transparency requirements
Despite the price transparency rule taking effect in January 2021, the Biden administration waited four months before CMS began taking any action, with the first batch of warnings issued in mid-April 2021.7 Even so, only a handful of hospitals received warnings in this first month of action—a lackluster start to price transparency enforcement.
Unfortunately, enforcement has not substantially improved since this time, thanks in large part to CMS’s relaxed attitude towards enforcement. The “warnings” issued by CMS are typically followed by months of silence before the agency follows up. On average, it takes CMS 185 days—or roughly six months—to follow up with a corrective action plan request after a warning is issued.8 In some cases—such as with The HSC Pediatric Center in Washington, D.C.—it took nearly a year for CMS to follow up with a corrective action plan request.9
Unsurprisingly, monetary penalties are the exception rather than the rule, with just four hospitals facing fines by CMS.10 Even when fines are issued, the amounts are so insignificant that hospitals can recoup the monetary assessments in as little as 40 minutes of patient revenue.11 And in the rare instances when fines are assessed on hospitals, it is only after months of noncompliance.12

Half—or fewer—of the cases initiated by CMS reach the point of a request for a corrective action plan.13-14 In most other instances, CMS simply issues a warning and then provides hospitals with more than enough runway to eventually comply at a time convenient for hospital administrators.15
From minimal fines to long delays, CMS has demonstrated a consistent lack of seriousness in its enforcement of hospital price transparency requirements.
Price transparency enforcement timelines by CMS are wildly inconsistent
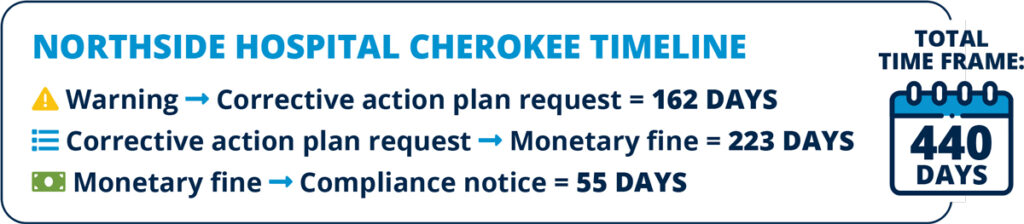
Unfortunately, even when CMS does take action, the timeframes to force hospitals to comply are wildly inconsistent. Case resolutions take an average of 251 days—or more than eight months. This ranges from as few as 63 days (such as in the case of Lake Huron Medical Center in Michigan) to as many as 487 days (such as in the case Mount Sinai Beth Israel Hospital in New York).16
Even though a request for a corrective action plan can prolong the life of a case, this far from fully explains all the discrepancies. For example, in May 2021, Concord Hospital in Concord, New Hampshire received a warning, followed by a corrective action plan request 162 days later, and a case closure 76 days after that—for a total of 238 days or nearly eight months.17 Just 30 miles down the road in Laconia, its branch of Concord Hospital was simply given a warning—no corrective action plan request—yet took a total of 279 days from start to finish to achieve compliance.18 The issues with the hospital without the corrective action plan should have been resolved more quickly, but it actually took nearly 20 percent longer.19

Across the country, CMS has created a patchwork of inconsistent enforcement timeframes that has resulted in similarly situated hospitals being afforded different amounts of time for compliance.
CMS is stonewalling full access to hospital price transparency records
In March 2022, FGA filed a Freedom of Information Act (FOIA) request with CMS to uncover its actions with respect to warnings, notices of violations, corrective action plan requests, and penalties issued in relation to hospital price transparency.20 After months of delays from CMS, the agency failed to provide any responsive documents—prompting FGA to file a lawsuit against the agency in August 2022 to obtain these crucial documents.21
In November 2022, a federal judge sided with FGA and ordered CMS to hand over all documents pertaining to FGA’s FOIA request by April 2023.22 While FGA began receiving documents in January 2023, FGA received a letter from CMS in March indicating their intention to withhold the bulk of the documents—nearly 34,000 pages—under the “trade secret” exemption of FOIA law.
The absence of the overwhelming majority of the responsive documents has prevented a full and complete understanding of CMS’s actions to address price transparency violations. To date, the records received by FGA only represent approximately one-third of the warnings CMS has claimed to have issued, one-half of the corrective action plans CMS has claimed to have requested, and one-half of the fines CMS has claimed to have imposed.23 These missing records prevent a full analysis of case closure timeframes and processes, as well as conceal certain scrutinized hospitals from the public’s view.
Mediation to determine whether these withheld materials should be released to FGA is scheduled for mid-July 2023.
CMS’s blocking of the overwhelming majority of responsive documents is an attempt to stonewall the public’s view of how the agency has addressed price transparency violations. Ironically, CMS has displayed the same stunning lack of transparency in their unresponsiveness to FGA’s FOIA request as hospitals have displayed in response to federal price transparency rules.
BOTTOM LINE: CMS is willfully ignoring hospital price transparency violations
From slow-rolling enforcement actions and issuing minimal fines to only reviewing a fraction of hospitals with potential violations, CMS has made it clear that they are not concerned with price transparency violations. CMS’s refusal to turn over tens of thousands of pages of records only underscores their failure to commit to full transparency.
CMS should release as many responsive documents as possible, and Congress should continue to place pressure on the agency to be more transparent in its enforcement of federal hospital price transparency rules.
In the meantime, states should take matters into their own hands by imposing state-level price transparency requirements. For example, in 2023, the Arkansas State Legislature passed and Governor Sarah Sanders signed into law legislation that will require the Department of Health to fine hospitals that have been found in violation of federal requirements.24
America’s hospitals must be transparent with their consumers—but that requires CMS to finally step up and do its job.
REFERENCES
1 Centers for Medicare & Medicaid Services, “Medicare and Medicaid programs: CY 2020 hospital outpatient PPS policy changes and payment rates; Ambulatory surgical center payment system policy changes and payment rates; Price transparency requirements for hospitals to make standard charges public,” Federal Register 84(229): 65,524 (2019), https://www.govinfo.gov/content/pkg/FR-2019-11-27/pdf/2019-24931.pdf.
2 American Hospital Association v. Azar, 468 F. Supp. 3d 372 (D.D.C. 2020), https://scholar.google.com/scholar_case?case=18069046475700227215.
3 Hayden Dublois and Jonathan Ingram, “How America’s hospitals are hiding the cost of health care,” Foundation for Government Accountability (2022), https://thefga.org/research/americas-hospitals-are-hiding-the-cost-of-healthcare.
4 Author’s calculations based on data provided by a data services company that collects hospitals’ price information on 6,387 hospitals in all 50 states and the District of Columbia. Hospitals that post a complete machine-readable file with negotiated rates, including both cash prices and private plan negotiated rates, were considered compliant for this analysis. This may overstate the number of hospitals that are compliant with the transparency rule as it did not consider whether hospitals had posted a consumer tool for shoppable services. Data was accessed in June 2023.
5 Patient Rights Advocate.Org, “Fourth semi-annual hospital price transparency report,” Patient Rights Advocate.Org (2023), https://www.patientrightsadvocate.org/february-semi-annual-compliance-report-2023.
6 Rebecca Pifer, “House Republicans target Biden admin over hospital price transparency noncompliance,” Health Care Dive (2023), https://www.healthcaredive.com/news/republicans-target-biden-hospital-price-transparencycompliance/650480.
7 Author’s analysis based on hospital price transparency records obtained by FGA from CMS.
8 Ibid.
9 Ibid.
10 Centers for Medicare & Medicaid Services, “Hospital price transparency enforcement updates,” U.S. Department of Health and Human Services (2023), https://www.cms.gov/newsroom/fact-sheets/hospital-price-transparencyenforcement-updates.
11 Hayden Dublois and Jonathan Ingram, “How America’s hospitals are hiding the cost of health care,” Foundation for Government Accountability (2022), https://thefga.org/research/americas-hospitals-are-hiding-the-cost-of-healthcare.
12 Author’s analysis based on hospital price transparency records obtained by FGA from CMS.
13 Ibid.
14 Centers for Medicare & Medicaid Services, “Hospital price transparency enforcement updates,” U.S. Department
of Health and Human Services (2023), https://www.cms.gov/newsroom/fact-sheets/hospital-price-transparencyenforcement-updates.
15 Author’s analysis based on hospital price transparency records obtained by FGA from CMS.
16 Ibid.
17 Ibid.
18 Ibid.
19 Ibid.
20 Hayden Dublois and Jonathan Ingram, “How America’s hospitals are hiding the cost of health care,” Foundation for Government Accountability (2022), https://thefga.org/research/americas-hospitals-are-hiding-the-cost-of-healthcare.
21 FGA, “FGA files lawsuit against the Biden administration’s Centers for Medicare and Medicaid Services (CMS) for stonewalling requests regarding hospital price transparency,” Foundation for Government Accountability (2022), https://thefga.org/press/fga-lawsuit-biden-cms-hospital-price-transparency.
22 FGA, “Judge orders Biden’s CMS to stop evading lawful requests for hospital price transparency records,” Foundation for Government Accountability (2022), https://thefga.org/press/judge-biden-cms-stop-evading-requestshospital-price-transparency.
23 Author’s comparison of received CMS documents to CMS’s public analysis. See, e.g., Centers for Medicare & Medicaid Services, “Hospital price transparency enforcement updates,” U.S. Department of Health and Human Services (2023), https://www.cms.gov/newsroom/fact-sheets/hospital-price-transparency-enforcement-updates.
24 Arkansas Legislature, “Act 482,” State of Arkansas (2023), https://www.arkleg.state.ar.us/Bills/Detail?id=HB1452&ddBienniumSession=2023%2F2023R.
