Maximize Enrollment, Weaken Program Integrity: How the Biden Administration’s Proposed Medicaid Rule Would Decimate an Already Broken Program
Key Findings
- The Medicaid program was created as a safety net for the truly needy but has strayed from its original purpose.
- The Medicaid program is already full of waste, fraud, and abuse, and the Biden administration’s proposed rule would make it even worse.
- The proposed rule would further handcuff states’ ability to manage their Medicaid programs.
- Weakened program integrity measures have led to skyrocketing enrollment during the public health emergency, and the proposed rule would only further drive up enrollment.
Background
The Medicaid program was designed to provide a safety net for truly needy Americans, including low-income children, individuals with disabilities, and seniors needing long-term care.1 But over the decades, the Medicaid program has strayed from its original purpose.
Medicaid eligibility has expanded numerous times over the years—with the focus shifting to maximizing enrollment, rather than serving the truly needy.2 In 2000, enrollment sat at 34 million.3 By February 2020, enrollment had catapulted to 74 million, more than doubling over two decades.4 But after the Medicaid handcuffs were locked onto states, enrollment exploded at an even morerapid rate. Enrollment currently sits at a record-high 97 million and could reach 100 million by January 2023.5
But as Medicaid has grown, program integrity has progressively gotten weaker as Medicaid has become riddled with waste, fraud, and abuse.6 Even worse, the truly needy—those the program was designed to serve—have been pushed to the back of the line.7
With the Medicaid program in shambles, the federal government should take steps to correct the issue. But instead of seeking solutions, the Biden administration proposed a rule that would only create additional problems.
The Medicaid Program Is Already Full of Waste, Fraud, and Abuse—And the Biden Administration’s Proposed Rule Would Only Make It Worse
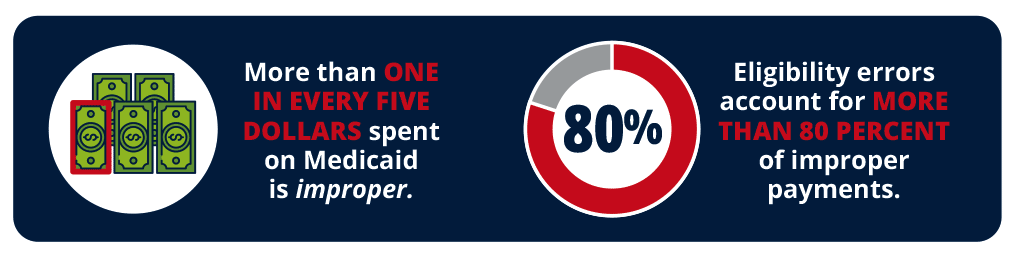
As the Medicaid program has ballooned in size, so have the long-running program integrity issues. More than one in every five dollars spent on Medicaid is improper, most of which are from eligibility errors, administrative oversights, and fraud.8 Eligibility errors account for more than 80 percent of improper payments, resulting in countless ineligible enrollees receiving benefits.9
State and federal audits have shined light on the problems plaguing the Medicaid program— namely, ensuring that only those eligible for the program are receiving benefits. In California, auditors found that more than 4.3 million enrollees were ineligible, or potentially ineligible.10 And in New York, auditors found that more than one million enrollees were ineligible or potentiallyineligible.11 Audits in other states have produced similar results.12
Even more shocking, audits have identified tens of thousands of individuals that were enrolled multiple times in the same state.13 In some cases, individuals had as many as seven different Medicaid cases open at one time.14 And auditors have found hundreds of thousands of Medicaid enrollees that are enrolled in multiple states.15 In some cases, the duplicative enrollment is the result of identity theft. Auditors found more than 20,000 enrollees with high-risk identities in Arkansas—including some with stolen or fraudulent Social Security numbers.16 In New Jersey, auditors found more than 18,000 enrollees with fake or duplicate Social Security numbers.17
Making matters worse, state Medicaid agencies have difficulty verifying the eligibility status of incarcerated or deceased applicants. In Arkansas, Louisiana, Missouri, and Ohio, auditors uncovered millions of dollars paid to cover the cost of care for inmates—despite inmates being ineligible for Medicaid.18 Auditors have also discovered hundreds of millions of Medicaid dollars spent on deceased individuals, some of whom had been dead for 40 years.19
These problems have resulted in massive program integrity issues in Medicaid. As a result of waste, fraud, and abuse, improper payments account for more than 40 percent of all federal Medicaid spending growth since 2013.20 If the Biden administration’s proposed rule goes into effect, even more ineligible enrollees will flood the Medicaid program, making matters worse.
The Biden Administration’s Proposed Rule Would Further Handcuff States
In 2012, the Obama administration issued rules that limited states’ ability to perform redeterminations in Medicaid.21 States were limited to only performing redeterminations once per year for certain eligibility groups.22 And the Biden administration is now doubling down by proposing a rule that would expand these same restrictions to all eligibility groups.23
Currently, states are required to conduct redeterminations at least once a year—a commonsense measure, as changes in life circumstances can occur throughout the year.24 But the Biden administration would take the current minimum and make it the new maximum, limiting states to conducting redeterminations not more than once a year for all eligibility groups.
The proposed rule would further handcuff states by severely limiting how states can perform redeterminations and verify eligibility. For example, states would be prohibited from performing face-to-face interviews for eligibility checks, despite the rise in identity theft in welfare.25
The rule would also force states to keep ineligible cases open for months as part of a “reconsideration period,” and then accept late, outdated information from applicants to determine eligibility.26 States’ ability to verify certain information—such as address or citizenship—would be impaired.27 And even worse, states would not be allowed to request financial follow-up information if the initial data indicates a person could be eligible.28

The Biden administration’s proposed rule would not only make it more difficult for states to manage their Medicaid programs, but also fuel the already surging program enrollment.
Enrollment Skyrockets When Redeterminations Are Performed Infrequently
During the height of the pandemic, Congress provided states with a small increase in their Medicaid funding through the Families First Coronavirus Response Act.29 But unfortunately, the increased funding came with massive strings attached.30 By accepting the funds, states were prohibited from strengthening eligibility standards or removing ineligible enrollees from the program.31

The Medicaid handcuffs were the driving force behind a massive enrollment surge.32 Because of the handcuffs, enrollment is at an all-time high of 97 million—and is rapidly approaching 100 million enrollees.33 More than 90 percent of enrollment growth resulted from Medicaid lock- ins—and an estimated 21 million enrollees that are ineligible but cannot be removed from the program.34 This skyrocketing enrollment more than outweighs the small funding boost provided by the federal government, and as a result, taxpayers are being drained for more than $16 billion each month—just to cover ineligible enrollees.35
If the Biden administration’s proposed rule goes into effect, states can expect more of the same. The proposed rule introduces a new set of handcuffs designed to hold back redeterminations and limit the effectiveness of eligibility standards. Recent history has shown that this is a recipe for disaster.
Congress Should Rein in Biden’s Spending Spree With the REINS Act
President Biden is unilaterally trying to make these Medicaid program changes through the proposed rule, despite no statutory authority to do so.36 This proposed rule is the latest in a long line of unilateral and unlawful regulations issued by the current administration.37 Since taking office, President Biden has launched a record-shattering regulatory spending spree, issuingmore costly rules than any other president in modern history.38
Unsurprisingly, the recent proposed CMS rule comes at a high cost to state and federal taxpayers.39 By CMS’s own calculations, the proposal would cost at least $100 billion over the next five years— though the actual cost would likely be much higher.40
Congress should have a say over massive new regulatory spending. To do so, federal lawmakers should pass the Regulations from the Executive in Need of Scrutiny (REINS) Act and require legislative approval of major rules—rules carrying a price of $100 million or more. Congress can follow the lead of states like Florida and require legislative approval for costly rules before they are implemented.41
THE BOTTOM LINE: The Medicaid program is already in shambles, and without intervention, the Biden administration’s proposed rule will only make matters worse.
President Biden is on an out-of-control spending spree. This record-shattering spree caused cumulative regulatory costs to continue to climb up to a shocking $1.1 trillion.42 These regulatory actions are not only draining limited taxpayer resources, but also now threaten the ability of states to strengthen the integrity of their welfare programs.
Fortunately, lawmakers have a simple solution. Congress should pass the REINS Act and require congressional approval of costly rules before they are implemented. This would curb the Biden administration’s out-of-control regulatory spree and help prevent further costly changes to the Medicaid program.
REFERENCES
1 Centers for Medicare and Medicaid Services, “Program history,” U.S. Department of Health and Human Services (2022), https://www.medicaid.gov/about-us/program-history/index.html.
2 Jonathan Ingram and Sam Adolphsen, “Stopping the Medicaid madness: How congress and states can start salvaging some program integrity,” Foundation for Government Accountability (2022), https://thefga.org/paper/stopping-the-medicaid-madness-how-congress-and-states-can-start-salvaging-some-program-integrity/.
3 Ibid.
4 Ibid.
5 Ibid.
6 Hayden Dublois and Jonathan Ingram, “Ineligible Medicaid enrollees are costing taxpayers millions,” Foundation for Government Accountability (2022), https://thefga.org/paper/ineligible-medicaid-enrollees-costing-taxpayers-billions/.
7 Nic Horton, “Waiting for help: The Medicaid waiting list crisis,” Foundation for Government Accountability (2018), https://thefga.org/paper/medicaid-waiting-list/.
8 Hayden Dublois and Jonathan Ingram, “Ineligible Medicaid enrollees are costing taxpayers billions,” Foundation for Government Accountability (2022), https://thefga.org/paper/ineligible-medicaid-enrollees-costing-taxpayers-billions.
9 Ibid.
10 Sam Adolphen, et al., “Comment on proposed streamlining Medicaid eligibility rule,” Opportunity Solutions Project (2022), https://solutionsproject.org/resources/comment-on-proposed-streamlining-medicaid-eligibility-rule/.
11 Ibid.
12 Ibid.
13 Ibid.
14 Ibid.
15 Ibid.
16 Ibid.
17 Ibid.
18 Ibid.
19 Ibid.
20 Ibid.
21 Centers for Medicare and Medicaid Services, “Medicaid program: Eligibility changes under the Affordable Care Act of 2010,” U.S. Department of Health and Human Services (2012), https://www.federalregister.gov/documents/2012/03/23/2012-6560/medicaid-program-eligiblity-changes-under-the-affordable-care-act-of-2010.
22 Ibid.
23 Centers for Medicare and Medicaid Services, “Streamlining the Medicaid, Children’s Health Insurance Program, and Basic Health Program application, eligibility determination, enrollment, and renewal processes,” U.S. Department of Health and Human Services (2022), https://www.federalregister.gov/documents/2022/09/07/2022-18875/streamlining-the-medicaid-childrens-health-insurance-program-and-basic-health-program-application.
24 42 C.F.R. § 435.916 (2021), https://www.ecfr.gov/current/title-42/chapter-IV/subchapter-C/part-435/subpart-J/subject-group-ECFR0717d3fdf4a090c/section-435.916.
25 Alli Fick and Jonathan Ingram, “Top five unemployment insurance fraud schemes—And how to stop them,” Foundation for Government Accountability (2021), https://thefga.org/paper/top-five-ui-fraud-schemes.
26 Centers for Medicare and Medicaid Services, “Streamlining the Medicaid, Children’s Health Insurance Program, and Basic Health Program application, eligibility determination, enrollment, and renewal processes,” U.S. Department of Health and Human Services (2022), https://www.federalregister.gov/documents/2022/09/07/2022-18875/streamlining-the-medicaid-childrens-health-insurance-program-and-basic-health-program-application.
27 Ibid.
28 Ibid.
29 Jonathan Ingram and Sam Adolphsen, “Stopping the Medicaid madness: How Congress and states can start salvaging some program integrity,” Foundation for Government Accountability (2022), https://thefga.org/paper/stopping-the-medicaid-madness-how-congress-and-states-can-start-salvaging-some-program-integrity/.
30 Ibid.
31 Ibid.
32 Ibid.
33 Ibid.
34 Ibid.
35 Ibid.
36 Sam Adolphen, et al., “Comment on proposed streamlining Medicaid eligibility rule,” Opportunity Solutions Project (2022), https://solutionsproject.org/resources/comment-on-proposed-streamlining-medicaid-eligibility-rule/.
37 Alli Fick, et al., “Congress must rein in President Biden’s regulatory spending spree to tame inflation,” Foundation for Government Accountability (2022), https://thefga.org/paper/congress-must-rein-spending-to-tame-inflation/.
38 Ibid.
39 Sam Adolphen, et al., “Comment on proposed streamlining Medicaid eligibility rule,” Opportunity Solutions Project (2022), https://solutionsproject.org/resources/comment-on-proposed-streamlining-medicaid-eligibility-rule/.
40 Ibid.
41 Haley Holik, “Why Florida is a national model for regulatory reform,” Foundation for Government Accountability (2022), https://thefga.org/paper/florida-is-a-national-model-for-regulatory-reform/.
42 Alli Fick, et al., “Congress must rein in President Biden’s regulatory spending spree to tame inflation,” Foundation for Government Accountability (2022), https://thefga.org/paper/congress-must-rein-spending-to-tame-inflation/.
