Arkansas’s Medicaid Meltdown: How Bad Policies Have Led to Busted Budgets and Skyrocketing Enrollment
Key Findings
- Medicaid enrollment is already at an all-time high and still rising.
- Arkansas's private option model has caused massive enrollment overruns and busted budgets.
- The private option model has failed in every other state.
- Pandemic-related policies have caused Arkansas's Medicaid dilemma to get worse.
Overview
The Medicaid program was designed to offer a helping hand to truly needy Americans—vulnerable populations such as seniors, pregnant women, low-income children, and people with disabilities.1 But the program has drastically deviated from its original purpose.
As a result, the Medicaid program is reeling. Nationwide enrollment sits at an estimated 98 million—a record high—and is on track to surpass 100 million in early 2023.2 Rather than focusing on the truly needy, federal and state lawmakers have opted to open the eligibility doors to able-bodied adults—most of whom are not working and do not have children.3
While these problems have existed for years, pandemic-related policies only made the situation worse, with millions of ineligible enrollees now siphoning resources away from the truly needy.4 Over the last three years, states were barred from removing ineligible enrollees from their programs due to the federal Medicaid handcuffs.5 But states will soon be able to begin the removal process starting April 1, 2023, and state officials should move aggressively to remove ineligible enrollees.6 This will help protect taxpayers and ensure resources are available for those in true need.
In Arkansas, skyrocketing Medicaid enrollment and busted budgets have become impossible to ignore.7 Without a significant shift, Arkansas’s Medicaid program will continue to serve as a stark warning to both expansion and non-expansion states alike.
Medicaid Expansion Has Been Draining Arkansas’s Resources for Years
In 2013, Arkansas took the bait and expanded Medicaid under ObamaCare.8 In doing so, Arkansas began offering benefits to a new class of able-bodied adults.9
But Arkansas’s approach is different from other expansion states around the country.10 Arkansas utilizes the “private option,” a model that provides able-bodied adults with private health insurance plans purchased through the ObamaCare exchange and paid for with Medicaid dollars.11 The private option prioritizes able-bodied adults by providing them with better coverage than it provides to truly needy Arkansans, and it is also bleeding taxpayers dry.12
Original enrollment estimates claimed that only 250,000 able-bodied adults would be eligible for benefits under the private option model.13 But by 2022, there were nearly 340,000 able-bodied adults enrolled in Medicaid in Arkansas—an enrollment overrun of 36 percent.14
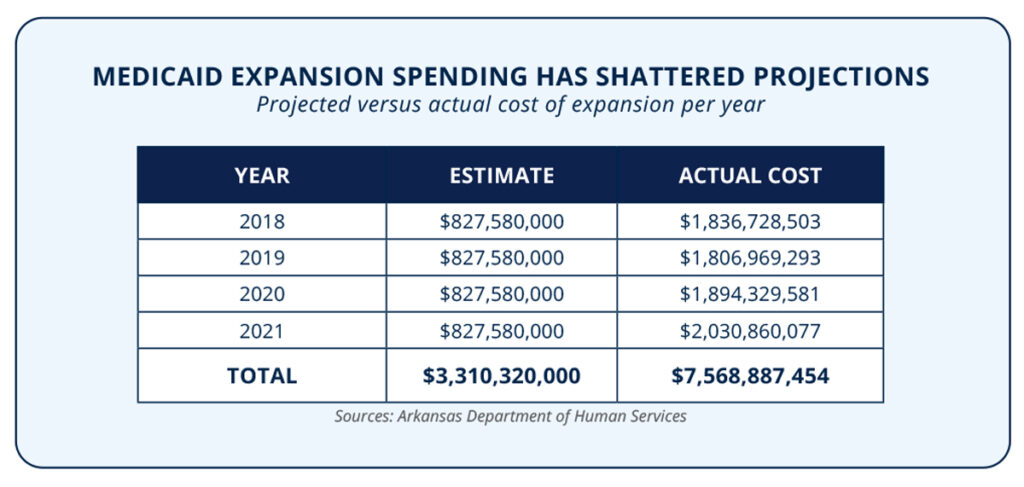
Similarly, state officials initially estimated that Medicaid expansion would cost taxpayers $1.8 billion over the first three years.15 But two and a half years later, cost overruns had already reached 79 percent.16 Even worse, state officials projected that expansion costs could reach $6 billion from 2014 through 2021.17 But unsurprisingly these estimates were inaccurate at best and misleading at worst. In fact, according to the Arkansas Department of Human Services, Medicaid expansion has already cost more than $10 billion since 2018—a cost overrun of 67 percent.
18Since 2013—the year before expansion was implemented in Arkansas—Medicaid’s share of the budget as a percent of total expenditures has grown by 33 percent.19 In 2022, more than one in every four taxpayer dollars in Arkansas were spent on Medicaid—with expansion costing nearly $2.5 billion through November.20-21 All told, Medicaid spending in Arkansas has ballooned by 60 percent since the year before expansion.22
While traditional Medicaid expansion leads to cost overruns and busted budgets, the private option model used by Arkansas is even worse.23 An analysis by the Arkansas Department of Human Services concluded that the cost of coverage for private option enrollees was $661 per member per month—compared to just $260 for Medicaid enrollees receiving standard fee for service benefits.24 The Government Accountability Office conducted an analysis of Arkansas’s private option and found that “questionable methods” were used to make the proposal seem budget neutral—even though it could cost state taxpayers nearly $1 billion more than a conventional expansion model.25
Overall, the Medicaid situation in Arkansas is dire. According to the most recent data, more than one in three state residents are receiving Medicaid benefits, creating an expensive culture of dependency statewide.26 The private option model only exacerbates the problem, which has caused other states to scrap it.
Other States Have Followed Arkansas’s Lead—And the Private Option Failed
Only two other states have followed the Arkansas private option model of expansion—and both states abruptly ended the program due to mounting costs and a lack of insurers.27
In 2014, Iowa implemented a version of the private option that allowed able-bodied adults to purchase expansion benefits through the ObamaCare exchange.28 Unsurprisingly, less than a year later, the state ended the private option due to skyrocketing premiums and insolvent carriers.29 Indeed, one of the state’s two expansion insurers recorded a loss of $163 million in 2014 alone, citing expansion as the reason.30 Facing similar issues, the other insurer pulled out and stopped accepting expansion enrollees altogether.31
New Hampshire also experimented with a private-option-style expansion, but it was short lived.32 After costs began to skyrocket, the legislature scrapped the waiver, and the state transitioned to conventional Medicaid expansion.33 State estimates indicated that by eliminating the private option, the program’s costs would decrease by more than half.34
The jury is not out on the private option—only three states have implemented this style of expansion, and two have rejected it due to rising costs and a lack of solvent insurance carriers. Arkansas has been facing similar issues for years but has not yet rejected the failed model.
Unfortunately, Arkansas’s Medicaid woes do not stop there. Pandemic-related policies placed a pair of handcuffs on states around the country, and Arkansas was not immune.
Congressional Handcuffs Have Made Arkansas’s Medicaid Woes Even Worse
As part of the Families First Coronavirus Response Act, Congress offered states a temporary increase to their traditional Medicaid funding.35 But this additional funding came with massive strings attached, as states had to surrender control over portions of their Medicaid programs.36 In exchange for the small funding boost, states were barred from removing any enrollee from Medicaid, even those that the state knows are ineligible or committed fraud, unless the person left the state or voluntarily opted out of the program.37
As a result, Medicaid enrollment exploded, reaching an estimated 98 million in December 2022—an all-time high.38Even more shocking, there are an estimated 22 million enrollees that do not meet eligibility criteria—resulting in nearly one in four Medicaid enrollees nationwide being ineligible for benefits.39 Costing an estimated $18 billion per month, these ineligible enrollees are draining taxpayers and siphoning limited resources away from the truly needy.40
In Arkansas alone, there are an estimated 1.2 million people enrolled in Medicaid—with more than 205,000 ineligible enrollees as of December 2022.41 Ineligible enrollees are costing state taxpayers nearly $22 million per month, far more than is covered by the additional funding provided by the federal government.42
Unsurprisingly, federal bureaucrats are encouraging states to slow walk removing ineligible enrollees. Bureaucrats are suggesting that states take up to 14 months to wrap up the process—as well as encouraging states not to perform eligibility reviews on more than 11 percent of their total caseload a month.43 But state officials should aggressively remove ineligible enrollees as soon as possible to preserve limited resources for the truly needy.
If Arkansas is to rebound from the problems plaguing their Medicaid program, state officials must take an aggressive approach to the redetermination and removal process.
THE BOTTOM LINE: To regain control of its Medicaid program, Arkansas must reassess the private option model. State officials should also move aggressively to remove ineligible enrollees from the program.
Arkansas’s Medicaid problems are multipronged. By expanding Medicaid, Arkansas opened the door to massive enrollment hikes and uncontrollable costs. And by opting to use the private option model, these problems were only compounded. Making matters worse, congressional handcuffs left Arkansas officials without the ability to strengthen eligibility standards or remove ineligible enrollees.
Fortunately, states may restart eligibility checks on February 1, 2023, and begin removals on April 1, 2023.44Arkansas officials should move aggressively to remove ineligible enrollees as soon as possible. Despite federal bureaucrats encouraging states to take more than a year to finish the process, Arkansas taxpayers and the truly needy deserve better.
State lawmakers must also reassess the utility of the private option and determine whether Medicaid expansion is still right for Arkansas.
These commonsense steps are urgently needed to address the Medicaid mishaps hurting the Natural State, and without action, the situation is only poised to get worse.
REFERENCES
1 Centers for Medicare & Medicaid Services, “CMS’ program history,” U.S. Department of Health and Human Services (2021), https://www.cms.gov/About-CMS/Agency.Information/History#:~:text=Though%20Medicare%20and%20Medicaid%20started,affordable%20health%20care%20they%20need.
2 Author’s calculations based upon data provided by the U.S. Department of Health and Human Services and state Medicaid agencies on total Medicaid enrollment between February 2020 and the most recent month available, trended forward to December 2022 with each state’s geometric average annual enrollment growth since February 2020.
3 Sam Adolphsen and Jonathan Ingram, “Stopping the Medicaid madness: How Congress and states can start salvaging some program integrity,” Foundation for Government Accountability (2022), https://thefga.org/research/stopping-the-medicaid-madness-how-congress-and-states-can-start-salvaging-some.program-integrity.
4 Ibid.
5 Ibid.
6 Michael Greibrok, “How Congress and states can rein in Biden bureaucrats while protecting taxpayers’ money and Medicaid program integrity,” Foundation for Government Accountability (2022), https://thefga.org/research/how.congress-states-can-rein-biden-bureaucrats.
7 Jonathan Bain and Hayden Dublois, “Arkansas’s private option model is costing more than twice as much as conventional Medicaid expansion,” Foundation for Government Accountability (2021), https://thefga.org/research/arkansas-private-option-cost.
8 Ibid.
9 Ibid.
10 Ibid.
11 Ibid.
12 Ibid.
13 Division of Medical Services, “Arkansas draft 1115 waiver for public comment,” Arkansas Department of Human Services (2013),
14 Arkansas Department of Human Services, “Monthly enrollment and expenditures report calendar year 2022,” Arkansas Department of Human Services (2022), https://humanservices.arkansas.gov/wp-content/uploads/Monthly.Enrollment-and-Expenditure-Report_September-2022.pdf.
15 Jonathan Ingram and Nic Horton, “A budget crisis in three parts: How ObamaCare is bankrupting taxpayers,” Foundation for Government Accountability (2018), https://thefga.org/research/budget-crisis-three-parts-obamacare.bankrupting-taxpayers.
16 Ibid.
17 Department of Human Services, “Estimated Medicaid-related impact of the ACA with expansion,” State of Arkansas (2012), https://web.archive.org/web/20160805224301/http://humanservices.arkansas.gov/director/Documents/Updated%20c ost%20estimates%20for%20Medicaid%20expansion%20Nov%202012.pdf.
18 Author’s calculations based on monthly enrollment and expenditure reports from 2018 through 2022, provided by the Arkansas Department of Human Services.
19 Author’s calculations based on Medicaid’s share of total expenditures in FY2000 and FY2022, provided by the National Association of State Budget Officers.
20 Brian Sigritz et al., “2022 state expenditure report,” National Association of State Budget Officers (2022), https://higherlogicdownload.s3.amazonaws.com/NASBO/9d2d2db1-c943-4f1b-b750.0fca152d64c2/UploadedImages/SER%20Archive/2022_State_Expenditure_Report_-_S.pdf.
21 Department of Human Services, “Monthly enrollment and expenditures report calendar year 2022,” State of Arkansas (2022), https://humanservices.arkansas.gov/wp-content/uploads/Monthly-Enrollment-and-Expenditure-Report_November-2022-AM.pdf.
22 Author’s calculations based on total Medicaid spending in FY2000 and FY2022, provided by the National Association of State Budget Officers.
23 Jonathan Bain and Hayden Dublois, “Arkansas’s private option model is costing more than twice as much as conventional Medicaid expansion,” Foundation for Government Accountability (2021), https://thefga.org/research/arkansas-private-option-cost.
24 Ibid.
25 Ibid.
26 Author’s calculations based upon total state Medicaid enrollment and the most recent Census Bureau population estimates.
27 Jonathan Ingram, “Arkansas’s so-called conservative approach to ObamaCare expansion has failed,” Foundation for Government Accountability (2018), https://thefga.org/research/arkansas-conservative-obamacare-expansion-has.failed.
28 Ibid.
29 Ibid.
30 Ibid.
31 Ibid.
32 Ibid.
33 Ibid.
34 Ibid.
35 Hayden Dublois et al., “Millions of ineligible enrollees come at a high cost to states,” Foundation for Government Accountability (2022), https://thefga.org/research/ineligible-medicaid-enrollees-high-cost.
36 Ibid.
37 Michael Greibrok, “How Congress and states can rein in Biden bureaucrats while protecting taxpayers’ money and Medicaid program integrity,” Foundation for Government Accountability (2022), https://thefga.org/research/how-congress-states-can-rein-biden-bureaucrats.
38 Author’s calculations based upon data provided by the U.S. Department of Health and Human Services and state Medicaid agencies on total Medicaid enrollment between February 2020 and the most recent month available, trended forward to December 2022 with each state’s geometric average annual enrollment growth since February 2020.
39 Author’s calculations based upon data provided by a proprietary microsimulation model that incorporates data on monthly Medicaid enrollment disaggregated by state, per capita monthly costs disaggregated by state and eligibility group, the distribution of ineligible enrollees at annual redetermination disaggregated by eligibility group, states’ blended FMAP rate based on the distribution of expected ineligibles due to lock-ins, and the share of new enrollment attributable to reported lock-ins disaggregated by state.
40 Ibid.
41 Ibid.
42 Ibid.
43 Centers for Medicare and Medicaid Services, “Letter promoting continuity of coverage and distributing eligibility and enrollment workload in Medicaid, the Children’s Health Insurance Program (CHIP), and Basic Health Program (BHO) upon conclusion of the COVID-19 public health emergency,” U.S. Department of Health & Human Services (2022), https://www.medicaid.gov/federal-policy-guidance/downloads/sho22001.pdf.
44 Michael Greibrok, “How Congress and states can rein in Biden bureaucrats while protecting taxpayers’ money and Medicaid program integrity,” Foundation for Government Accountability (2022), https://thefga.org/research/how-congress-states-can-rein-biden-bureaucrats.
